We Need Class, Race, and Gender Sensitive Policies to Fight the COVID-19 Crisis
Luiza Nassif-Pires, Laura de Lima Xavier, Thomas Masterson, Michalis Nikiforos, and Fernando Rios-Avila
Disproving the belief that the pandemic affects us all equally, data collected by New York City Department of Health and Mental Hygiene and a piece published today in the New York Times shows that the novel coronavirus is “hitting low-income neighborhoods the hardest.”[1] In a forthcoming policy brief, we share evidence that this pattern would be the case and provide a solid explanation as to why (Nassif-Pires et al., forthcoming). Moreover, as we argue, the death tolls are also likely to be higher among poor neighborhoods and majority-minority communities. This inequality in health costs is in addition to an unequal distribution of economic costs. In short, poor and minority individuals are disproportionately feeling the impacts of this crisis. A concise version of our evidence is presented here.
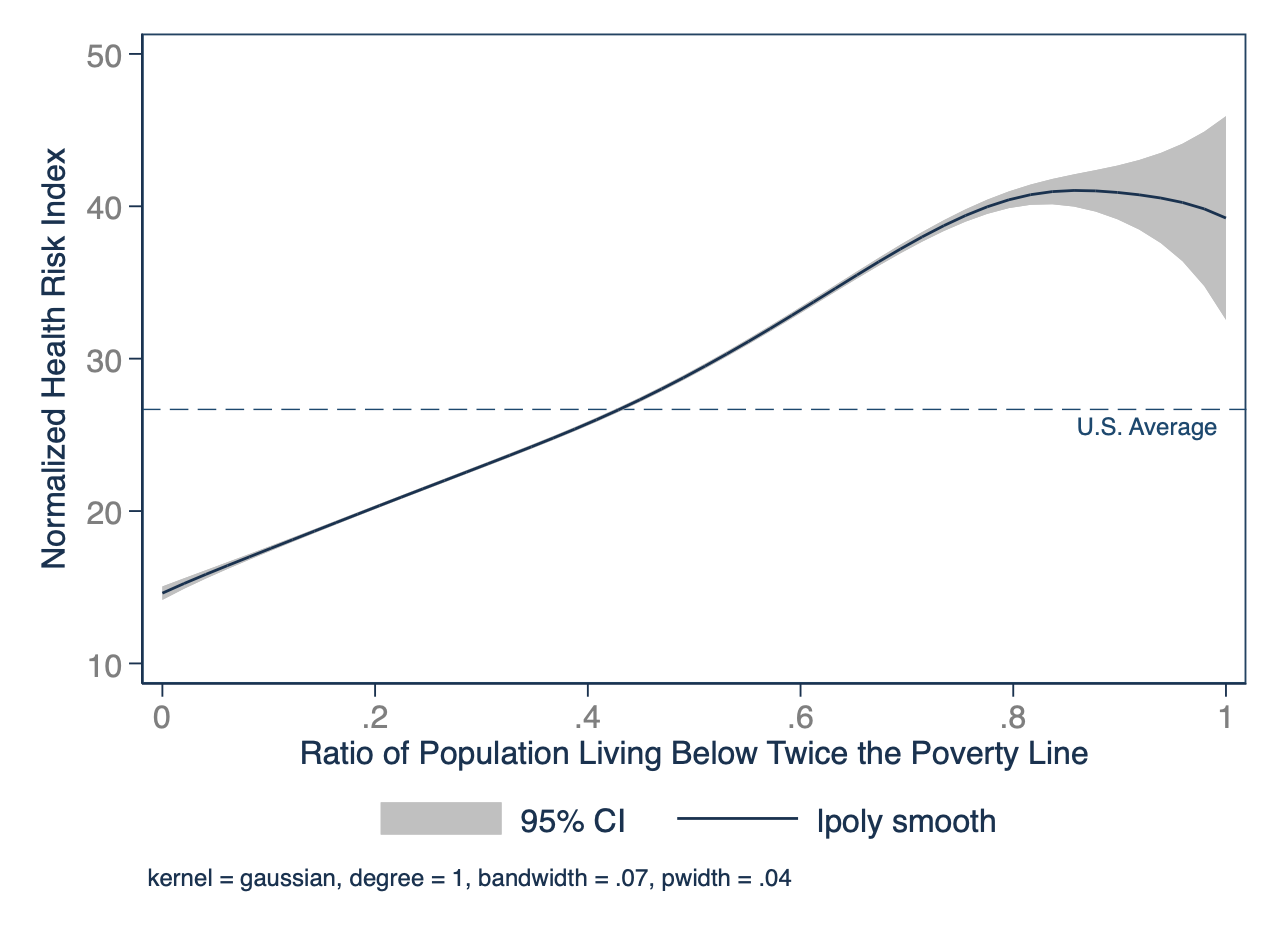
The toll of social inequality in healthcare is well known. A clear relationship has been repeatedly demonstrated between social determinants — such as income, education, occupation, social class, sex, and race/ethnicity — and the incidence and severity of many diseases. This association holds true for infectious respiratory illnesses such as influenza, SARS and also for COVID-19, as figure 1 shows. The consequences of this imbalance are particularly catastrophic when there is a massive disease outbreak. The precise mechanisms by which social determinants drive unequal disease burden during these outbreaks is harder to assess. On the one hand, there is a strong association of social determinants with clinical risk factors for respiratory illnesses such as chronic diseases, on the other, social aspects of poverty increase the risks of individuals contracting infectious diseases.
To establish the relationship between poverty and the clinical risk of a severe case of COVID-19, we estimate a health risk index as a function of poverty and percentage of minority population in neighborhoods of 500 cities. We use data from the 500 Cities project and from the American Community Survey. The risk index accounts for the incidence of chronic obstructive pulmonary disease, diabetes, coronary disease, cancer, asthma, kidney disease, high blood pressure, percentage of smokers, proportion of individuals with poor physical health and the proportion of the population that is above 65 years old. All data is available at the census tract level and results are presented in figure 1 and figure 2[2].
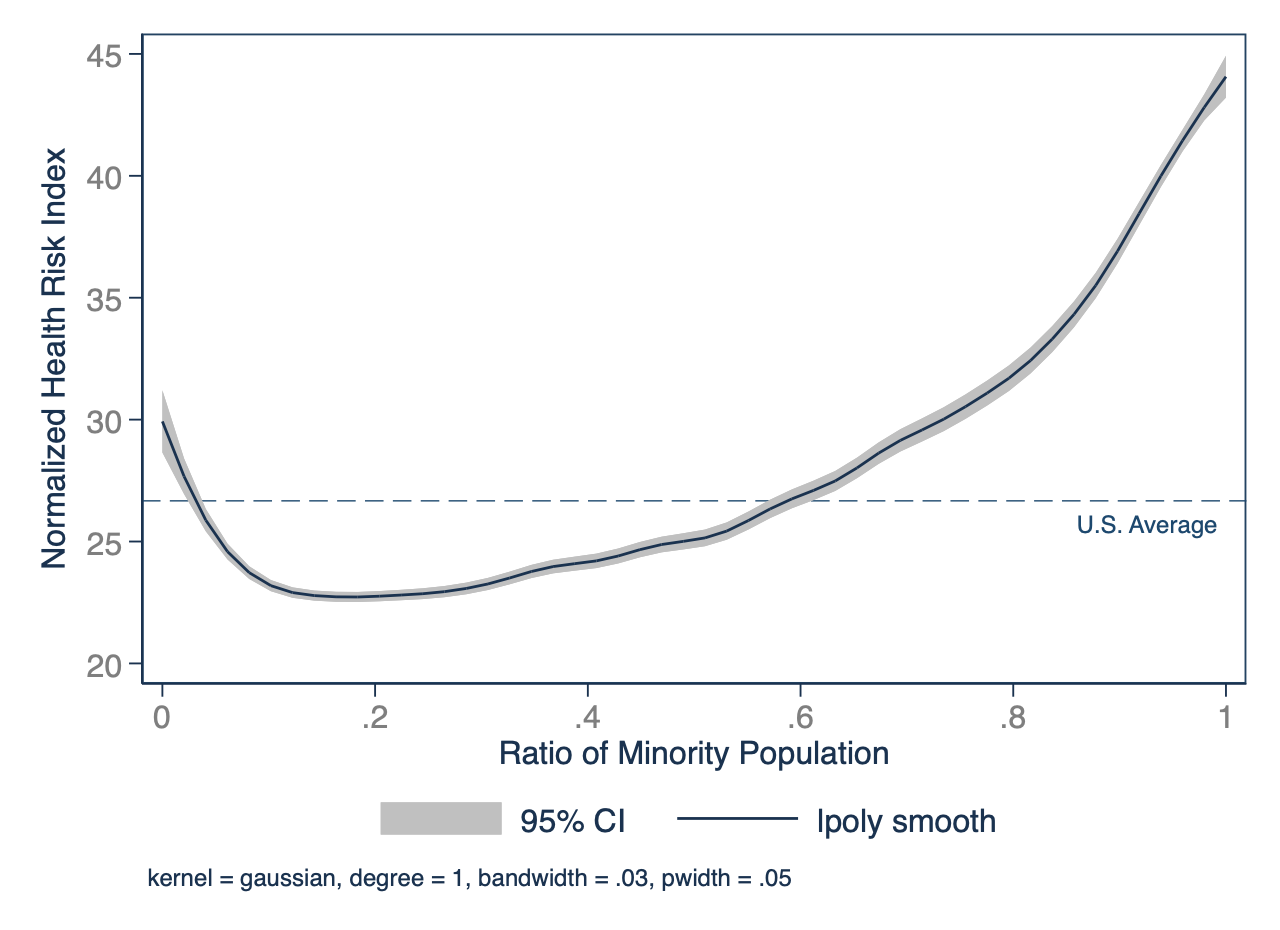
As figure 1 shows, the incidence of risk factors is much higher in poor communities. In neighborhoods with a higher percentage of the population living below two times the poverty line, the risk factor index is above the national average, while neighborhoods where no one lives under poverty present risk below average. At least one of these chronic diseases included in our risk index were reported in one fourth of COVID-19 cases and were even more prevalent in cases requiring intensive care and resulting in death. Chronic obstructive pulmonary disorders for instance have been shown to raise this risk of severe COVID-19 in 2.6-fold, and diabetes and hypertension by about 60% (Guan, W., Liang et al, 2020). Not surprisingly, these comorbidities also disproportionately affect socioeconomic minorities, making these populations alarmingly vulnerable to COVID-19, as illustrated in figure 2.
Figure 1- Estimated Health Risk by Share of Population in Poverty by Census Tract (US, 2017)
Source: Authors calculation using American Community Survey data retrieved from IPUMS (2020) and from the 500 cities Project (2019).
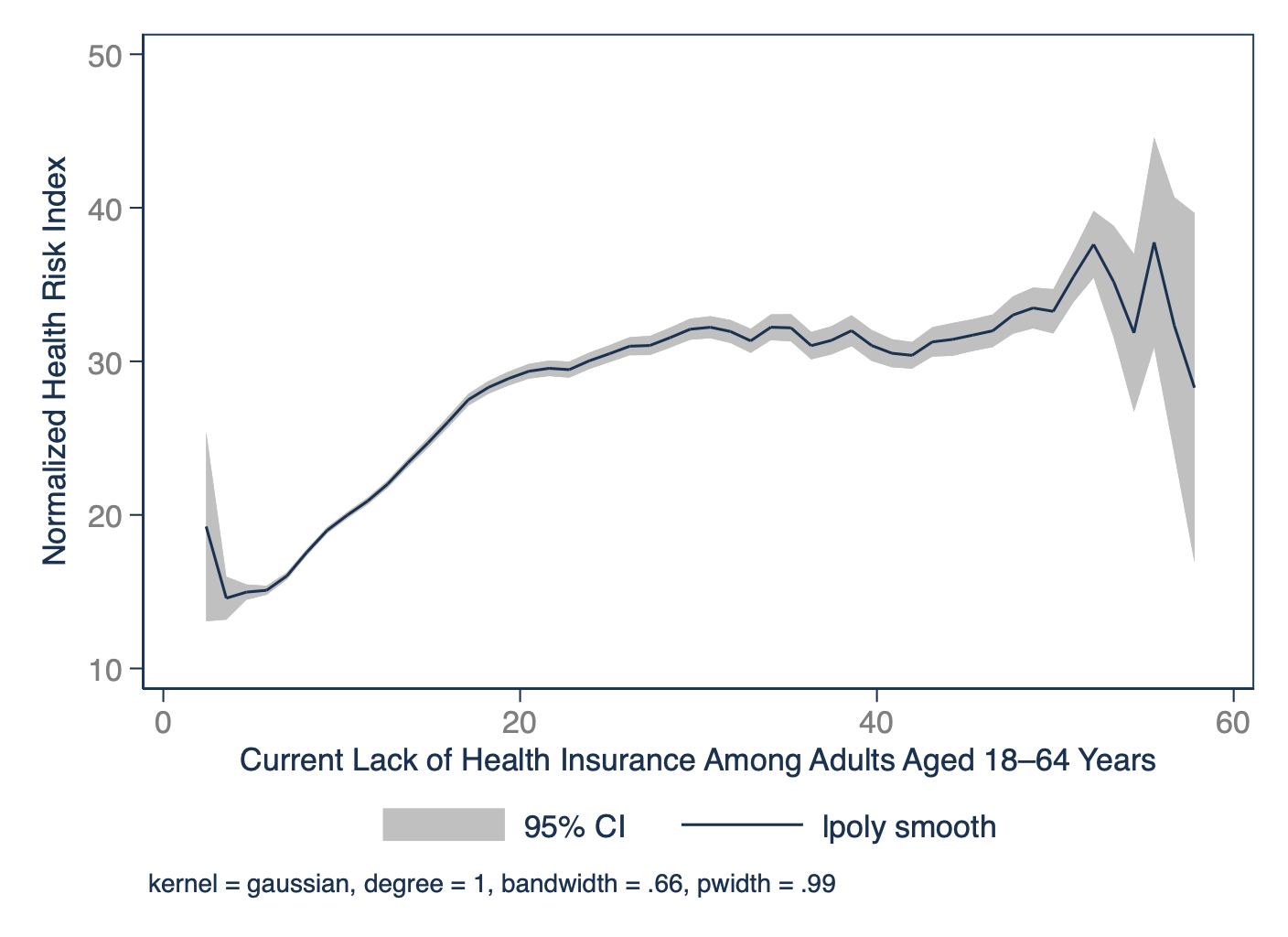
Furthermore, there is reason to believe that the health effects of being socioeconomically disadvantaged extend far beyond these clinically recognized risk factors. Studies that combine data from previous infectious respiratory pandemics provide strong evidence that the increased risk in this population might be largely driven by factors such as disproportionate access to healthcare and other differences in living and work conditions (Lowcock et al., 2012; Mamelund, 2017). Uninsured people are less likely to seek early treatment, making the lack of health insurance in the US another risk of severe cases of COVID-19. The lack of health insurance, another aspect of poverty, is also more prominent in areas where the population has higher health risk indexes (figure 3) adding yet one more layer of vulnerability for the population in poor communities. Similarly, during the 2009 H1N1 pandemic, socially disadvantaged populations showed increased prevalence of hospitalization, illness severity, and mortality both in the US and abroad (Tricco et al., 2012). In the US, however, neighborhood disadvantage, absence of sick leave policies in the workplace, and opposition to school closings were shown to be key social determinants of influenza transmission and illness with clinical risk only partially mediating this effect (Lowcock et al., 2012; Cordoba and Aiello, 2016). Similar imbalances were also found during the 2003 outbreak of Severe Acute Respiratory Syndrome (SARS-CoV) which is genetically related to the current SARS-CoV-2 causing COVID-19. In Hong Kong, the most severely hit city, an investigation on the influence of socioeconomic status and the spread of of SARS found a significant negative correlation between the incidence of SARS and median income levels (Bucchianeri, 2010). This correlation was primarily driven by differences in living conditions such as living in housing complexes with higher usage of public transportation, communal facilities and a higher number of floors and therefore elevator sharing. Investigations in the US and in Sweden during the 1918 influenza pandemic also demonstrated that the education, occupation, and home ownership were related to mortality (Grantz et al., 2016; Bengtsson, Dribe and Eriksson, 2018). At the extreme end of vulnerability, homeless people are at increased risk of contracting infectious diseases in crowded spaces, and more likely to develop severe symptoms because of underlying medical conditions and limited access to health care. In cities with a large population of homeless people, the effects of COVID-19 could be disastrous. https://nyti.ms/2IA1j5r
The prevalence of chronic respiratory disorders— an identified risk factor for severe COVID-19— is also sharply higher among the poor and in African American communities. This imbalance is present in both children and adults, and is predominantly attributed to environmental exposures, such as exposure to tobacco smoke, crowding and stress (Margolis et al., 1992; Hedlund, Eriksson and Rönmark, 2006; Pawlińska-Chmara and Wronka, 2007). In the state of New Jersey, asthma rates in African American children can be twice as high as their peers, and are determined by whether children live in a “black” zip code, with racial differences in incidence of asthma completely disappearing when correcting for their address (Alexander and Currie, 2017). These studies demonstrate a clear relationship between respiratory health problems and socioeconomic inequalities such as environmental segregation and residential racism, and serve as a warning of the devastating effect of that inequality during viral respiratory pandemics. Unfortunately figure 2 indicates that similar perverse results are likely to happen during a covid-19 epidemic.
Gender inequalities also result in unequal health and economic vulnerability, with women being at higher risk than men. Although initial reports from China suggested higher death ratios in men, women are both more likely to be exposed to viruses and to be responsible to care for those infected. Another worrisome piece of evidence from China is the observed increase in domestic violence[3] during the lockdown, which is already higher in lower income communities[4].
Figure 2 Estimated Health Risk by Minority Share of Population by Census Tract (US, 2017)
Source: Authors calculation using American Community Survey data retrieved from IPUMS (2020) and from the 500 cities Project (2019).
In summary, people who are socioeconomically disadvantaged are at increased risk of acquiring COVID-19 and of having worse outcomes, but are also the least likely to seek medical attention due to high out-of-pocket healthcare costs in the US. Approaches to tackling the health and economic effects of the pandemic that do not acknowledge and articulate with these factors will necessarily fail.
Figure 3 Estimated Health Risk by Lack of Health Insurance Among Adults Aged 18–64 Years by Census Tract (US, 2017)
Source: Authors calculation using American Community Survey data retrieved from the 500 cities Project (2019).
Policy Implications
Policies aimed at avoiding the uncontrolled spread of new pathogens in crowded and underserved areas start with our ability to develop tests and use them early on to identify infected people including mild cases in order to isolate them and track close contacts. For cities such as New York, Los Angeles and Seattle, it is far too late, but for many places, widespread testing integrated with social distancing policies are crucial. Such an approach was taken early on by South Korea and Hong Kong, but not in the United States. The failure in accurately tracking the spread of the virus is likely the reason for the high number of cases in New York. Data from China suggests that the disease is most easily spread between family members who are in frequent contact with one another (Huang et al., 2020). Moreover, the efforts of lockdown do not protect from infections within households, which also have a higher impact in poorer communities where more people share smaller spaces. Thus, the home quarantine model makes poor households even more vulnerable. Repurposing spaces such as hotels, gymnasiums and dorms to give individuals with mild infections or that have been in contact with cases the option of quarantining and recovering outside their homes can protect the lives of their families. This is especially important for individuals living in small apartments or houses and sharing space with vulnerable populations.
Two other distribution-sensitive policies that have potentially very large macroeconomic consequences at the moment are the provision of paid sick leave and access to healthcare. The recent stimulus bill includes provisions for paid sick-time, family, and medical leave. However, these provisions do not apply to employers with more than 500 employees, while small businesses with less than 50 employees can also ask for an exemption. As a result, only 25 percent of private sector employees are covered.[5] Access to paid leave decreases the rate of spread as it will keep individuals from going to work despite being ill. Therefore, we need to guarantee paid sick leave for everyone (part-time and gig-economy included), which should be subsidized by the government in the case of small businesses.
Access to healthcare has similar benefits. With the spread of the pandemic it has become abundantly clear that lack of access to healthcare can have important negative spillovers. People without access to healthcare not only get sick themselves (which is obviously important in its own right) but are also more likely to spread the virus to others. At this point, because of the structure of the US healthcare system, we face the paradox of people losing access to healthcare (mostly because they lose their jobs) at the time when they—but also the society and the economy as a whole—need it most. In order to mitigate the impact and the duration of the COVID shock, we need to have broad open access to testing for the coronavirus and treatment regardless of immigration and insurance status which should be cost-free to patients and without hidden costs. It is also important to extensively publicize to undocumented and uninsured individuals how to access free testing and treatment and encourage them to seek assistance as soon as needed to avoid an unnecessary increase in the risk of severity and in the rate of spread.
In addition to a freeze on foreclosures, there needs to be a nation-wide moratorium on eviction for at least the duration of the crisis. People are more likely to lack the funds to pay rent and so we would observe an increase in the homeless population, one of the most vulnerable groups. Furthermore, for individuals whose income were affected by Covid-19 and small businesses that closed, rent and utilities forgiveness should be granted, so we do not observe an increase in household indebtedness.
We need to provide child-care and/or school lunches at home for essential but low-paid workers whose children are now not going to school. A direct transfer payment of the kind contained in the stimulus package is a useful supplement to the above, but it should be on a monthly basis for the duration of the crisis rather than a one-time payment. All of these policies are necessary to ensure that those that are likeliest to be vulnerable to both the disease itself and the economic impacts, immediate and medium-term, are shielded from this disaster that they had no part in creating.
There needs to be an effort to map and design specific policies to protect highly vulnerable groups such as undocumented immigrants, the homeless population, inmates, victims of domestic violence, and the nursing home population, only to cite a few. Each of these groups requires a task force of its own to design appropriate policies.
This crisis also teaches us some lessons regarding policies for the medium run that would make us less vulnerable to crises. The lack of adequate access to healthcare for many Americans needs to be addressed. Some form of single-payer insurance, such as Medicare for all, would go a long way to removing the reluctance of individuals to seek care (anxiety about out-of-pocket costs, searching for in-network care providers, etc.), slowing the spread of future pandemics, as well as relieving budgetary pressure on states during crises resulting from their responsibility for funding Medicaid.
Finally, the increasingly high income inequality is one of the main structural problems of the US economy, and one of the main reasons for its recent poor macroeconomic performance (Nikiforos 2016, 2020). The stagnation of the wages over the last forty years is also one of the major explanations for the slowdown of productivity growth over the same period; labor being relatively cheap implies a weaker incentive to innovate and introduce labor-saving techniques of production. Unfortunately, neoliberal policies such as the financial deregulation, tax cuts to the wealthy, cuts on social spending by the Federal government and attacks on worker protections only reinforced this problem. Reverting these policies and strengthening our labor laws and unions can go a long way in addressing this issue.
A reduction in income inequality is one of the most important–if not the single most important—structural changes that needs to be implemented so that the US economy returns to a sustainable growth path in the medium run. Had these issues been addressed already, the impacts on the US of this pandemic would have been less severe. Maybe this time we can at least learn from our mistakes.
Luiza Nassif-Pires
Research Fellow, Levy Economics Institute. The author would like to thank Isabella Weber for insightful conversations and comments.
Laura de Lima Xavier
Department of Otolaryngology, Massachusetts Eye and Ear, Boston, MA, USA
Department of Neurology, Massachusetts General Hospital, Boston, MA, USA
Harvard Medical School, Boston, MA, USA
Thomas Masterson
Research Scholar, Levy Economics Institute
Michalis Nikiforos
Research Scholar, Levy Economics Institute
Fernando Rios-Avila
Research Scholar, Levy Economics Institute
References
500 Cities Project. https://www.cdc.gov/500cities/
Alexander D, Currie J. Is it who you are or where you live? Residential segregation and racial gaps in childhood asthma. J Health Econ. 2017 Sep;55:186–200.
Bengtsson T, Dribe M, Eriksson B. Social Class and Excess Mortality in Sweden During the 1918 Influenza Pandemic. Am J Epidemiol. 2018 Dec 1;187(12):2568–76.
Bucchianeri GW. Is SARS a Poor Man’s Disease? Socioeconomic Status and Risk Factors for SARS Transmission [Internet]. Vol. 13, Forum for Health Economics & Policy. 2010. Available from: http://dx.doi.org/10.2202/1558-9544.1209
Cordoba E, Aiello AE. Social Determinants of Influenza Illness and Outbreaks in the United States. N C Med J. 2016 Sep;77(5):341–5.
Department of Labor (DOL), News release: Unemployment Insurance Weekly Claims. March 26, 2020. https://www.dol.gov/ui/data.pdf, Accessed 12:00 March 26, 2020.
Fazzari, S. 2020. “The COVID-19 Recession: Unprecedented Collapse and the Need for Macro Policy”, Institute of New Economic Thinking Blog.
Grantz KH, Rane MS, Salje H, Glass GE, Schachterle SE, Cummings DAT. Disparities in influenza mortality and transmission related to sociodemographic factors within Chicago in the pandemic of 1918. Proc Natl Acad Sci U S A. 2016 Nov 29;113(48):13839–44.
Guan, W., Liang, W., Zhao, Y., Liang, H., Chen, Z., Li, Y., Liu, X., Chen, R., Tang, C., Wang, T., Ou, C., Li, L., Chen, P., Sang, L., Wang, W., Li, J., Li, C., Ou, L., Cheng, B., … He, J. (2020). Comorbidity and its impact on 1,590 patients with COVID-19 in China: A Nationwide Analysis. MedRxiv, 2020.02.25.20027664. https://doi.org/10.1101/2020.02.25.20027664
Hedlund U, Eriksson K, Rönmark E. Socio-economic status is related to incidence of asthma and respiratory symptoms in adults. Eur Respir J. 2006 Aug;28(2):303–10.
Huang, R. et al. (2020) ‘A family cluster of SARS-CoV-2 infection involving 11 patients in Nanjing, China’, The Lancet infectious diseases. doi: 10.1016/S1473-3099(20)30147-X.
IPUMS NHGIS, University of Minnesota, www.nhgis.org.
Lowcock EC, Rosella LC, Foisy J, McGeer A, Crowcroft N. The social determinants of health and pandemic H1N1 2009 influenza severity. Am J Public Health. 2012 Aug;102(8):e51–8.
Mamelund S-E. Social inequality – a forgotten factor in pandemic influenza preparedness [Internet]. Tidsskrift for Den norske legeforening. 2017. Available from: http://dx.doi.org/10.4045/tidsskr.17.0273
Margolis PA, Greenberg RA, Keyes LL, LaVange LM, Chapman RS, Denny FW, et al. Lower respiratory illness in infants and low socioeconomic status. Am J Public Health. 1992 Aug;82(8):1119–26.
Nassif-Pires, L., L. de Lima Xavier, T. Masterson, M. Nikiforos, and F. Rios-Avila. Forthcoming. “Pandemic of Inequality.” Public Policy Brief No. 149. Annandale-on-Hudson, NY: Levy Economics Institute of Bard College.
NY Times (2020) https://www.nytimes.com/2020/03/12/us/women-coronavirus-greater-risk.html
________(2020) https://nyti.ms/2IA1j5r
NY Times (2020) https://www.nytimes.com/interactive/2020/04/01/nyregion/nyc-coronavirus-cases-map.html?referringSource=articleShare
Oliveira, AN, Sages, L, Silva, G, Nassif-Pires, L. 2020 “Home Quarantine, Confinement with the abuser?” Multiplier Effect Blog.
Pawlińska-Chmara R, Wronka I. Assessment of the effect of socioeconomic factors on the prevalence of respiratory disorders in children. J Physiol Pharmacol. 2007 Nov;58 Suppl 5(Pt 2):523–9.
Tricco AC, Lillie E, Soobiah C, Perrier L, Straus SE. Impact of H1N1 on socially disadvantaged populations: systematic review. PLoS One. 2012 Jun 25;7(6):e39437.
[1] https://www.nytimes.com/interactive/2020/04/01/nyregion/nyc-coronavirus-cases-map.html?referringSource=articleShare
[2] For this exercise we perform a local polynomial regression between an estimated health risk index, constructed through principal component analysis, and the percentage of population living below two times the poverty line in census tracts, for figure 1, and between the health risk index and percentage of non-white population for figure 2. For details on the methodology or on the data please contact [email protected].
[3] https://www.sixthtone.com/news/1005253/domestic-violence-cases-surge-during-covid-19-epidemic
http://multiplier-effect.org/home-quarantine-confinement-with-the-abuser/
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5486977/
[5] From Bureau of Labor Statistics’ National Business Employment Dynamics Data by Firm Size Class, Table F. https://www.bls.gov/web/cewbd/table_f.txt, accessed March 30, 2020.



 ShareThis
ShareThis